At Caris Lifesciences, all of the stained slides went through a quality control process before they were able to leave the laboratory. Once out of the lab, they were looked at by a pathologist who put together a recommended treatment plan for rare and hard to treat cancers. They used a combination of immunohistochemical (IHC) stained slides, a molecular profile, and a comprehensive database of patient treatment. All of this was done in house, which helped Caris shine from the rest of the theragnostic labs.
As I progressed as a histotech, I learned more and more about looking at slides and stains to determine if things stained properly. I received training from pathologists, coworkers, and supervisors. If I had a question on a stain, I would always get the best answer I could from a supervisor. It was painstaking to learn it all, but it really helped me develop and understand and knowledge base of the stains we performed and also what a lot of tissue looks like under a microscope.

The majority of what I learned was developed when I was making tissue micro-arrays (TMA). Please see the section I’ve devoted to TMAs.
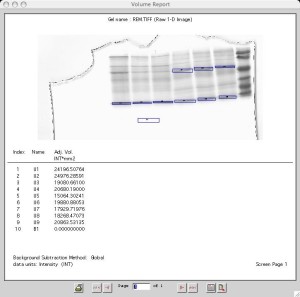
Quality control for the automated stainers (Ventana and Dako) consisted of looking at the TMA section placed on each slide. These act as positive controls for the stains. Several different tissue types were present that were know to stain positive for all of the stains. I was in charge of selecting tissue and passing the tissue by sectioning and staining each tissue type for all of the stains it was supposed to stain positive for. This was step one of the quality control process.

The final step before the slides were delivered to a pathologist was the QC stage. Someone would sit and look at the TMAs on each slide and also the tissue to make sure that it didn’t fall off and had a uniform stain. Sometimes in microtomy a section can be placed on a slide that is thick on one side and thin on the other, or had chatter or other anomalies. Once this was done, the case was logged and sent out of the lab. I spent a lot of days at the QC station. It was always a nice change of pace from the frustrating microtomy or monotonous staining procedures. It was fascinating to see all the different types of tumors and stains.